GM e log
Nov,01 2023
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
IMMANI AASRITHA
Roll no.49
8th semester
Nov 01, 2023
GENERAL MEDICINE
HOPI
pt was apparently asymptomatic 3 months back and developed a blister on the left great toe and that has ruptured and formed an ulcer which is not healed and that infection has gradually increased.
15 days back pt came to hospital with blackish discoloration of that great toe.
No h/o any fever
No h/o itching
No h/o vomitings ( at the time of joining)
PAST HISTORY:
Patient had similar complaints in the past 1 yr back for the right great toe and got amputated other outside hospital.
20 yrs back patient suddenly develoed blurring of vision for some time and rushed to a local hospital and found out that he had diabetes. (Diabetic since 20yrs )
Not a k/c/o HTN, ASTHMA, CVA, TB.
PERSONAL HISTORY:
Normal appetite
Mixed type of diet and irresistible eating of sweets.
Regular bowel and bladder movements
There are no allergies for food or any drugs
Addictions : patient used to drink and smoke daily in the past for 40 yrs and stopped10yrs back.
TREATMENT HISTORY:
50yrs back he got amputated his ring finger upto distal Interphalangeal joint because of trauma to that finger.
Since 20 yrs he is on oral metformin for diabetes.
2 yrs back he started taking insulin for diabetes.
1 yr back got amputated his right great toe.
FAMILY HISTORY:
His brothers have diabetes
VITALS
Temp: 98.7
Spo 2: 98%
Bp: 110/60 mm of hg
RR: 16cycles / min
Pulse: 66 bpm
GENERAL EXAMINATION:
Pt is well built and malnourished , well cooperative coherent and coordinative.
pallor : present
Icterus : absent
Cyanosis : absent
Clubbing : absent
Koilonochia : absent
Lymphadenopathy :absent
Pedal edema : mild
Mid arm circumference 28 cm
Mamc: 23.6 mm
Triceps skinfold thickness:14mm
Abdominal girth: 98cm
Fvf ratio: 98-23.6 =4.15
SYSTEMIC EXAMINATION
Cvs
S1S2 heard
No murmurs
Respiratory system:
Trachea central
Normal vesicular breath sounds heard
Cns :
No focal neurological deficits are observed
Per abdomen:
Scaphoid abdomen
No scars and sinuses
No organomegaly
Bowel sounds heard
LOCAL EXAMINATION:
Left leg
After rays amputation.
Healthy granulation tissue is seen.
Margins are regular.
No bleeding.
INVESTIGATIONS:
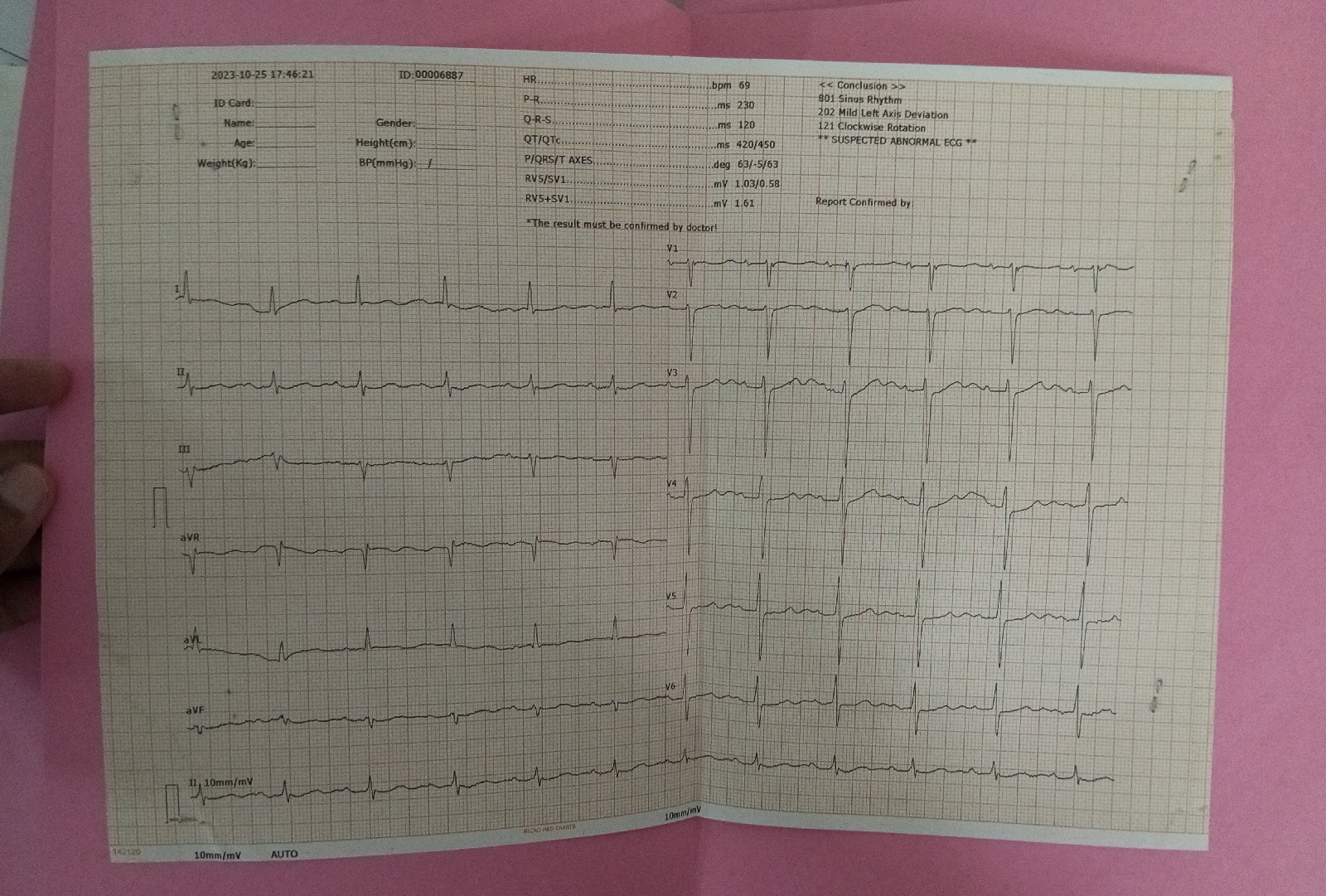
Ecg
25/10/2023
RFT
1) 30/10/2023
2) 25/10/2023
GLYCATED HAEMOGLOBIN
Prothrombin time
GLYCATED HAEMOGLOBIN
Blood sugar fasting
28/10/2023
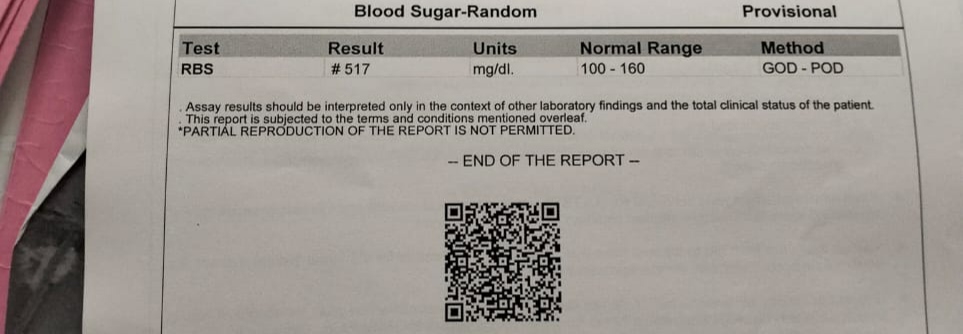
Random Blood sugar
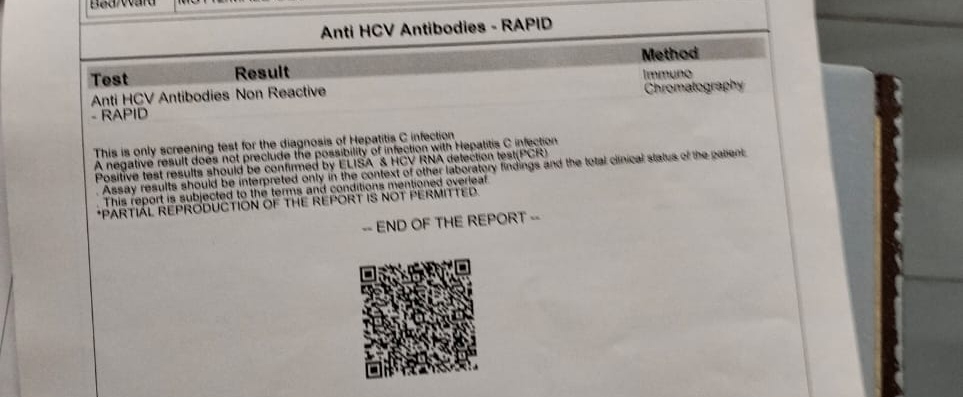
Serological tests
ABG
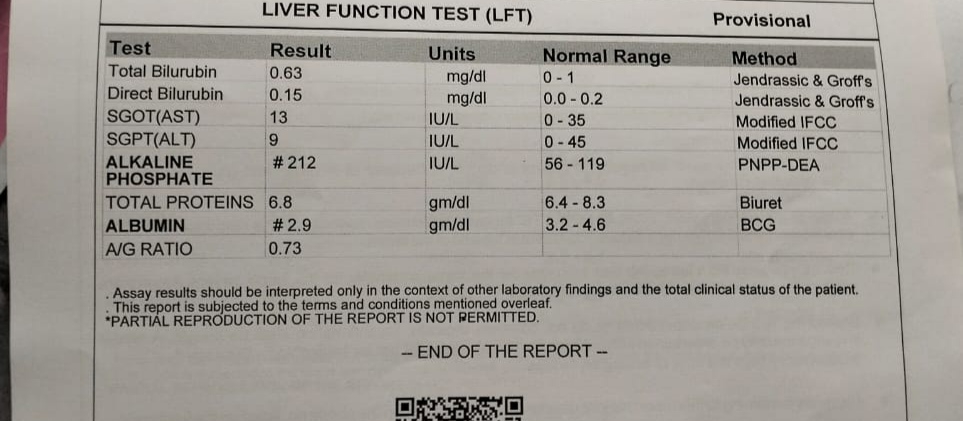
LIVER FUNCTION TEST
BLEEDING and CLOTTING TIME
Troponin
Complete urine examination
Liver function test
BLOODGROUPING AND RH TYPING
ULTRASOUND :
25/10/2023
27/10/2023
TREATMENT
26/10/23
Inj.Meropenem 1gm IV BD
Inj.Metrogyl 500mg IV TID
Inj.Pan 40mg IV OD
Inj tramadol 1 amp in 100 ml
Left lowerlimb elevation
Monitor Temp,PR,BP,SpO2 hourly
GRBS monitoring
liquid diet
27/10/23
Inj.Meropenem 1gm IV BD
Inj.Metrogyl 500mg IV TID
Inj.Pan 40mg PO OD
Tab linezolid 600mg PO OD
tab ultracet PO OD
tab atorvastatin 20mg
Tab ecospirin 325mg PO/ STAT
Inj.Atropine 0.6mg IV/STAT
Inj.HAI s/c TID
Left lowerlimb elevation
Monitor Temp,PR,BP,SpO2 hourly
GRBS monitoring
liquid diet
28/10/23
Inj.Meropenem 1gm IV BD
Inj.Metrogyl 500mg IV TID
Inj.Pan 40mg PO OD
Tab linezolid 600mg PO OD
Inj.Zofer 4mg IV/TID
tab ultracet PO OD
tab atorvastatin 20mg
Tab ecospirin 325mg PO/ STAT
tab.Clopidogrel 75mg PO/OD
Inj.Atropine 0.6mg IV/STAT
Inj.HAI s/c TID
Left lowerlimb elevation
Monitor Temp,PR,BP,SpO2 hourly
GRBS monitoring
liquid diet































Comments
Post a Comment