Nov15, 2023
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
IMMANI AASRITHA
Roll no.49
8th semester
Nov 15, 2023
GENERAL MEDICINE
CASE PRESENTATION
A 20 year old female labourer came with complaints of fever since 20 days facial and legs swelling since 20 days
complaints of throught pain SOB difficulty in swallowing since 3 days
HISTORY OF PRESENT ILLNESS
patient was apparently symptomatic 20 days back then developed fever which was insidious in onset gradually progressive high grade with chills and riger not relieving with medication facial puffiness on and off, legs swelling up to ankle associated with numbness, sob since 3 days Grade 2 MMRC relieved on rest not associated with chest pain , dyspecia since 3 days for both solids and liquids history of headache neck pain which is continuous not associated with vomitings history of facial puffiness one month back subsided by treatment given by local practitioner . Patient has ulcer over the back which is painful . no history of pain abdomen no burning maturation no difficulty in passing stool
History of loss of appittite
She is not a known case of diabetes hypertension asthma epilepsy thyroid disorders
PERSONAL HISTORY
As a mother of 3 children this patient wakes up at 5 am in the morning doing her daily chores in her house and sends her older 2 daughters to school and her husband to work she will do remaining chores and she will also goes to work as a daily or weekly labourer and comes home at 5pm to 8 pm based on work she had that day
Doing all these she neglected her food intake
Most of the time she skips her break fast and dinner some times she is eating rice with pickle only
She want to make sure that her daughters study well so she is working all the time
She married at the age of 15 yes and had her first child with in a year and in 1½ year she had another daughter and now she is having a 26 months baby
She didnt gave milk to all her child because she didn't produce milk
Since past few days she is having fever so that she didnt went to work stayed at home but she is doing her chores from past 4 days she is resting and did some of the chores only
GENERAL PHYSICAL EXAMINATION
Patient is conscious coherent co operative moderately built and nourished
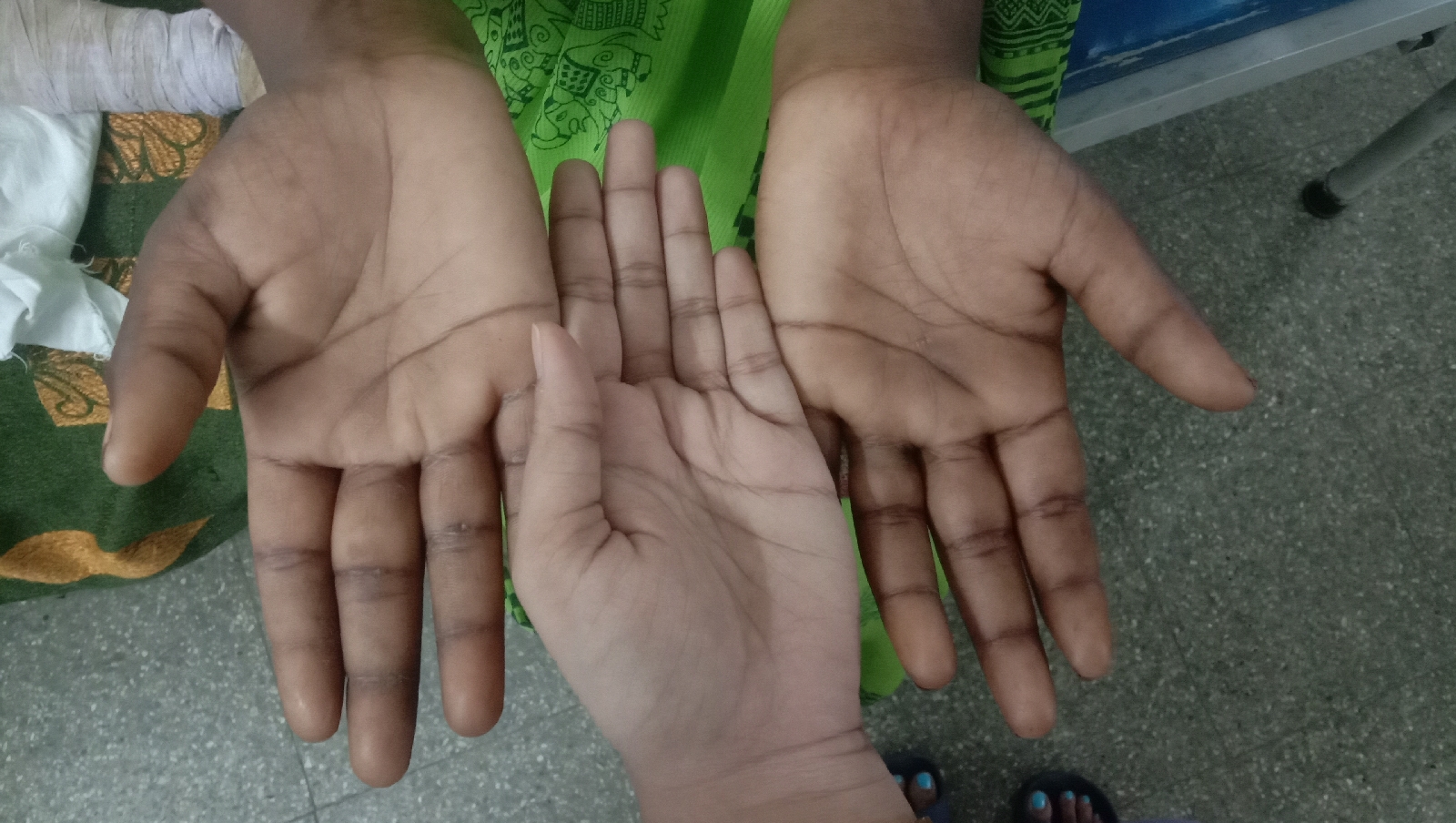
Pallor present
No icterus cyanosis clubbing pedal edema
Lymphadenopathy of bilateral lymph nodes are enlarged
She is having an abscess 1 to 2 weeks Back which was small in size initially and increased to 3 to 4 cms and after that her father applied some leaves on that then it opened and pus has came out of that
Systemic examination CVS : S1 S2 + no murmors
RS : BAE + , NVBS
CNS : no focal neurological deficits
P/A : soft non tender , no organomegaly
Oral cavity : Norma
Oropharynx : b/l anterior pillar congestion present
Right side tonsil grade I and left side tonsil grade II tonsilar hypertrophy present
Posterior pharyngeal wall : granular congestion present
PROVISIONAL DIAGNOSIS
Anemia
with tonsilalr hypertrophy
OSCE
Q . what are the possible causes of facial puffiness in this case
A . 1) anemia
2) the skin infection .. the molecular mimicry of the bacterial antigens with glomerular epithelial antigens causing glomerular deposition causing glomerulonephritis
3) the pharyngeal infection causing PSGN
Q. How can you confirm weather it is glomerular or due to anemia
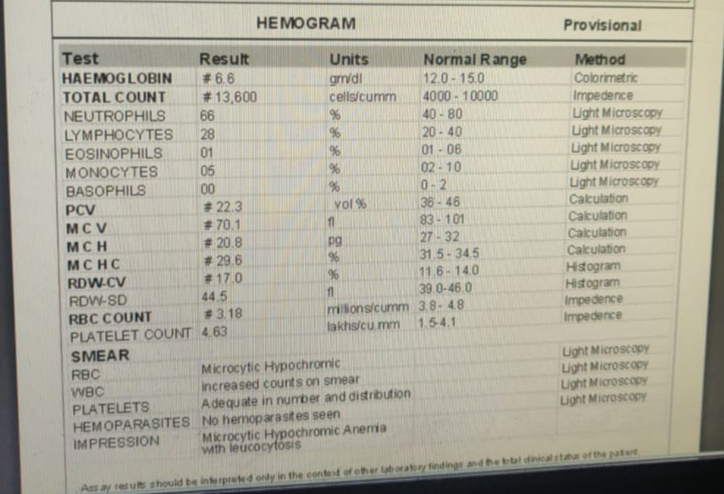
A . by checking the investigations of RFT, HEMOGRAM
In this patient
Here in this patient blood urea and serum electrolytes are normal except potassium levels for that we addes potclor to the patient
In hemogram shows that she is having anemia microcytic and hypochromic
Pointing towards iron deficiency anemia which is most common type of anemia in young Indian women.
Q. What if the RFT is not normal ? What should be your next investigation
A. Next investigation if RFT is deranged in this case is ASO titer bcz of PSGN
Q. What are the other investigations that are sent for this patient
A. Serology
Random blood sugar
X ray Chest
Q. Do you know why is alkaline phosphatate increased in this patient
A. Yes because of inflammation the alkaline phosphatase levels may be slight raised .
Q . what is the treatment give to this patient ?
A . INJ . LENIZOLID 650mg for 2 days and converted that into T. LENIZOLID 650 mg for next 5 days
Syp . POTCLOR 5ml in glass of water for 2 days
Tab. PARACETAMOL 650 mg po tid
Tab OROFER XT PO OD X 30 days
Q. Did you check the potassium levels after giving potclor
A . yes
SWOT analysis (Strengths, Weaknesses, Opportunities, Threats) of the patient's case:
Strengths:
She is on good attender care.
She has good support from family
She is getting better with the medication
Weaknesses:
1. Her financial status
2. Not eating proper meals and not eating on time
3 .
Opportunities:
1. Government is supplying free medication for the anemic women like her under anemia mukth bharat












Comments
Post a Comment